Weight Management:
A Comprehensive Overview
1. Introduction
Obesity is a complex, chronic disease associated with multiple comorbidities, including type 2 diabetes, cardiovascular disease, and certain cancers. Management requires a multidisciplinary approach tailored to individual patient needs.
2. Screening and Assessment
Before initiating treatment, a comprehensive assessment by your doctor usually includes:
BMI and Waist Circumference: Identify overweight (BMI ≥25) and obesity (BMI ≥30).
Medical Causes of Weight Gain: Rule out conditions such as:
Hypothyroidism
Cushing’s syndrome
Polycystic ovary syndrome (PCOS)
Menopause-related metabolic changes
Medications (e.g., antipsychotics, corticosteroids)
Eating Disorders Screening: Identify conditions such as binge-eating disorder or night-eating syndrome, which require specific interventions.
3. Lifestyle Management
3.1. Diet
An effective weight-loss diet should focus on sustainability and nutritional adequacy. Evidence-based dietary approaches include:
Mediterranean Diet: Emphasizes fruits, vegetables, whole grains, healthy fats, and lean proteins.
Low-Carbohydrate Diets (e.g., Keto, Atkins): May benefit individuals with insulin resistance but require monitoring.
Low-Fat Diets: Historically promoted but now considered less effective long-term.
Intermittent Fasting: Includes methods such as 16:8 or 5:2, showing benefits in some populations.
Portion-Controlled Diets (e.g., Meal Replacements): Useful in structured programs.
3.2. Exercise
Physical activity recommendations include:
Aerobic Exercise: 150–300 minutes per week of moderate-intensity activity (e.g., brisk walking, cycling).
Resistance Training: At least 2 sessions per week to preserve lean muscle mass.
High-Intensity Interval Training (HIIT): Effective for improving metabolic health and weight loss.
Other incidental physical activities is still important to burn calories (eg taking the stairs instead of the lifts)
4. Pharmacological Management
Pharmacotherapy is recommended for individuals with BMI ≥30 or BMI ≥27 with obesity-related comorbidities.
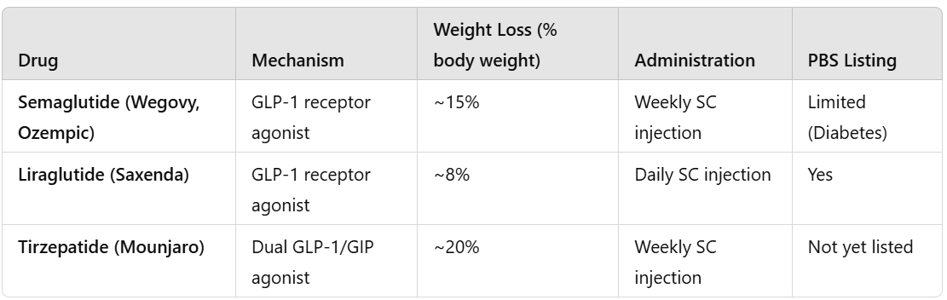
4.1. GLP-1 Receptor Agonists in Australia
GLP-1 receptor agonists have revolutionized weight management.
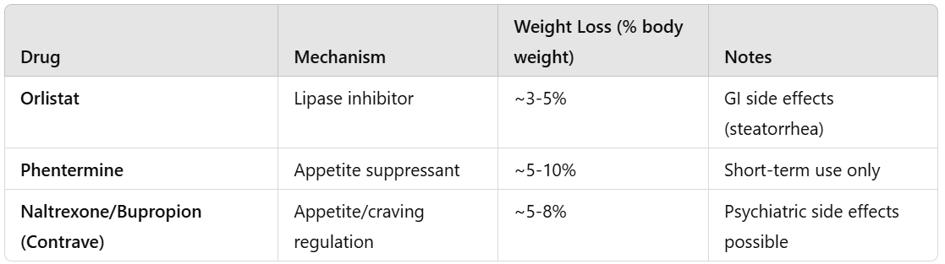
4.2. Other Pharmacological Options
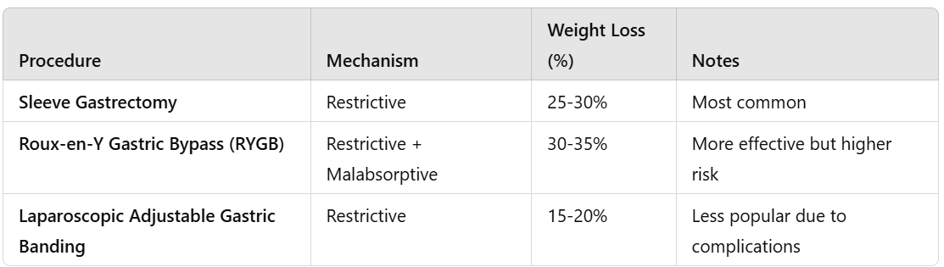
5. Surgical (Bariatric) Options
Bariatric surgery is recommended for:
BMI ≥40, or
BMI ≥35 with obesity-related comorbidities.
6. Multidisciplinary Approach
A team-based approach improves long-term outcomes:
Dietitian: Personalized meal planning.
Exercise Physiologist: Tailored exercise programs.
Psychologist: Address emotional eating and disordered eating patterns.
GP/Endocrinologist: Medical supervision and pharmacotherapy management.
Surgeon: For eligible patients considering bariatric surgery.
Conclusion
Effective weight management requires a holistic, patient-centered approach integrating lifestyle changes, medications, and surgery when appropriate. With new pharmacological advancements like semaglutide, tirzepatide, treatment options continue to evolve.
Resources
Austin weight control clinic: has many great videos and other resources